Update time:2025-10-14Visits:3264

Bao Chunde Professor of Rheumatology, Former Director of the Department of Rheumatology, Renji Hospital
Introduction
In an era when medical technology was still in its infancy, he dedicated himself with unwavering determination to pioneering new frontiers in medicine. Undaunted by challenges, he became a true trailblazer in his field.
With profound medical expertise and exceptional clinical skills, he brought renewed hope for recovery to countless patients with lupus erythematosus. Throughout his career in rheumatology research, he consistently broke from tradition, embraced innovation, and integrated science with humanistic care, developing groundbreaking treatment methods and philosophies.
Confronting the complex and often frustrating nature of rheumatic diseases, he never yielded. Through meticulous clinical observation and in-depth analysis, he introduced innovative diagnostic and therapeutic strategies that significantly improved accuracy and efficacy, delivering tangible benefits to patients.
This is the story of a medical pioneer whose extraordinary contributions to rheumatology have forged a legendary career.
The Path to Medicine
Those born in the 1950s experienced a period of profound societal transformation in China. They witnessed the nation’s journey from turmoil to stability and adapted to the changes brought by the “Reform and Opening-Up” era. Forged by the trials of their time, this generation developed resilience and wisdom—a deep appreciation for tradition coupled with an adaptability to rapid modernization, facing challenges with remarkable maturity and resolve.
“In our era, the economy was underdeveloped, and medicine was seen as an unattractive profession—it offered modest pay and limited social prestige. But from a historical perspective, I was fortunate. In 1978, the reinstatement of the national college entrance examination changed the destiny of a generation, and I was admitted to Shanghai Second Medical University, embarking on my journey in medicine. During those four years, as a young man, I absorbed a vast amount of medical knowledge and gradually came to understand the responsibilities and mission of being a doctor.”
In 1982, Bao Chunde graduated from Shanghai Second Medical University with a Bachelor of Medicine degree and began his internship at Renji Hospital.
“Looking back, I consider myself a veteran of Renji. From 1983 to this day, I have remained here. When I first started, the hospital was still called Shanghai Third People’s Hospital. I recall that our department’s equipment was rudimentary and the work environment was far from modern. Yet, this foundational period became an invaluable cornerstone of my career.”
Upon joining Renji Hospital, Bao Chunde, like other young physicians, began with foundational tasks. Despite the demanding workload and numerous challenges, he sustained his passion for medicine and his compassion for patients. Through hands-on clinical experience, he honed his practical skills and accumulated invaluable expertise.
It was then that Bao Chunde came to see medicine not merely as a science, but as an art—a highly interdisciplinary field requiring relentless learning, continuous reflection, and unwavering dedication.
Pioneering Rheumatology
In clinical practice, Bao Chunde quickly demonstrated exceptional potential. His diligence and perseverance captured the attention of senior specialists, particularly his outstanding performance in internal medicine. As the hospital explored new subspecialties, new opportunities opened up for him.
“When I first arrived at Renji, I noticed the rheumatology division within internal medicine. At the time, rheumatology was an emerging field. Many patients with complex conditions went undiagnosed or untreated in other departments and were eventually referred here. I saw immense potential and promise in this field. Although our unit initially had only a few beds and limited resources, nothing could impede our progress.”
Bao Chunde’s mentors—Professor Chen Shunle and Academician Jiang Shaoji—profoundly shaped his medical career. Academician Jiang Shaoji was a renowned gastroenterologist in China, while Professor Chen Shunle was a founding figure of Shanghai’s rheumatology community.
“Due to the political climate of the era, Professor Chen Shunle had not yet obtained the qualifications to be a postgraduate supervisor, yet he provided me with immense guidance and support. So, I took an indirect approach. In 1985, I enrolled as a graduate student under Academician Jiang Shaoji, but my de facto mentor was Professor Chen Shunle. Through this arrangement, I received systematic training in rheumatology.”
During his graduate studies, Bao Chunde gained precious learning opportunities. Under Professor Chen Shunle’s mentorship, he delved into various rheumatic diseases and their treatments. A towering figure in medicine, Professor Chen took a keen interest in Bao Chunde’s development, guiding his research and encouraging international academic exchange.
In an age before the internet, accessing the latest international medical literature was a challenge. Yet, Professor Chen Shunle frequently returned from conferences with cutting-edge research and foreign publications. These resources expanded Bao Chunde’s medical knowledge and laid a solid foundation for his future research.
Reflecting on the establishment of rheumatology at Renji Hospital, it was a pioneering move that underscored the hospital’s vision for medical innovation. As early as 1979, Renji founded its rheumatology department, becoming one of the first in China to do so, alongside Peking Union Medical College Hospital. This positioned Renji as a national leader in the field from its inception.
“Reflecting on the creation and growth of our department fills me with emotion. As one of the nation’s first, we shouldered the responsibility of pioneering the field. In those early days, rheumatology was in its infancy nationwide; infrastructure and techniques were far from mature. The challenges we faced were unprecedented.”
Initially, diagnostic and therapeutic resources were scarce. Immunological and serological tests were not widely available, and treatment options were limited. Yet, Bao Chunde and his team persevered. To improve diagnostic accuracy, they established a dedicated laboratory within the hospital, developing serological methods tailored for rheumatic diseases. These efforts boosted early diagnosis rates and enabled timely, effective treatment.
Advances in therapy were equally arduous. With fewer drugs and protocols available, the team relentlessly explored novel approaches. They collaborated with domestic and international research institutions on extensive clinical studies and boldly integrated traditional Chinese medicine with Western therapies, developing innovative drug regimens that renewed hope for patients.
By the late 1990s, as medical technology advanced and new drugs emerged, the department flourished. It established the nationally influential Institute of Rheumatology, founded the Sino-Australian Centre for Personalised Immunotherapy, and earned recognition as a National Key Clinical Specialty. These achievements were the culmination of decades of dedication by generations of rheumatologists at Renji.
From its humble beginnings to its current acclaim, Renji’s rheumatology department has remained steadfastly patient-centered, driving progress in the field.

Building Foundations Through Groundbreaking Research
Systematic research and clinical practice in lupus erythematosus have long been the cornerstone of Renji’s rheumatology department, driving breakthroughs across multiple domains.
As early as 1991, Bao Chunde tackled challenges in emergency treatment for systemic lupus erythematosus (SLE) by proposing innovative strategies. His work highlighted the critical role of emergency interventions, improving clinical practices and boosting patient survival and quality of life.
His team also conducted detailed clinical and serological analyses of juvenile-onset SLE, advancing personalized therapies for children and adolescents with rheumatic diseases. For rare conditions like SLE complicated by cryptococcal meningitis, their studies established diagnostic and therapeutic frameworks, enriching the clinical understanding of rheumatic diseases.
Despite advances in systemic lupus erythematosus (SLE) treatment, significant unmet needs persist. SLE’s complex and incompletely understood pathogenesis limits the effectiveness of conventional therapies. Against this backdrop, Bao Chunde collaborated with researcher Zhang Xiaoming from the Shanghai Pasteur Institute on a groundbreaking study. They discovered new potential for the established drug rapamycin in SLE treatment, opening fresh avenues—particularly in targeting specific immune cell subsets.
“Our research identified a unique cell subset in SLE patients: atypical memory B cells (AtMs). Using advanced flow cytometry and multiplex immunohistochemistry, we observed significantly elevated AtMs in SLE patients, with levels closely linked to disease activity. Notably, these AtMs heavily infiltrated kidney tissue in patients with lupus nephritis.”
Discovered in 1964 in Easter Island soil, rapamycin was initially used to prevent organ transplant rejection. Bao Chunde found that as an mTORC1-specific inhibitor, rapamycin potently suppressed AtMs. It blocked their generation, their differentiation into antibody-secreting plasma cells, and the production of autoantibodies—demonstrating potential in eliminating pathogenic B cells.
“This finding reveals rapamycin’s promise in SLE therapy. Unlike conventional B-cell-targeted treatments, rapamycin selectively acts on specific B-cell subsets, potentially sparing normal immune cells and offering better efficacy with fewer side effects. It presents a novel paradigm, and we will continue exploring its mechanisms and applications.”
This discovery heralded a new direction in SLE treatment.
Bao Chunde’s 2023 breakthrough in lupus nephritis (LN) treatment was equally transformative.
Treating SLE and its complication, LN—especially refractory LN—remains a major challenge. While glucocorticoids and immunosuppressants offer partial relief, many patients fail to achieve optimal outcomes, making novel strategies urgently needed.
Bao Chunde’s team made significant headway by investigating the potential of iguratimod (IGU)-based combination therapy for refractory LN.
Iguratimod (IGU), a China-developed innovative drug (Class 1.1), was launched in China (2011) and Japan (2012). Its unique chemical structure and proven efficacy in rheumatoid arthritis quickly earned it prominence in rheumatology.
Beyond rheumatoid arthritis, IGU’s immunomodulatory properties have been extended to other autoimmune diseases—including Sjögren’s syndrome, SLE, and ankylosing spondylitis—showcasing its broad clinical value.
IGU’s dual action—potent immunomodulation and comprehensive bone protection—sets it apart. It significantly reduces rheumatoid factor and anti-CCP antibody levels while preventing bone destruction and deformity, making it uniquely effective among DMARDs (disease-modifying antirheumatic drugs).
“Refractory lupus nephritis has long been a formidable challenge. Despite progress, many patients still struggle to achieve full remission. We recognized the need to improve existing protocols and explore new pathways. Thus, we turned to iguratimod (IGU).”
Bao Chunde’s preliminary study showed that adding IGU to conventional immunosuppressants significantly boosted remission rates in refractory LN patients. The trial included 26 patients continuing their prior therapies, with IGU added. At six months, the complete remission rate reached 42.3%, ultimately climbing to 50% during follow-up.
This outcome was pivotal, offering a new therapeutic option and highlighting IGU’s potential in refractory LN. Notably, steroid doses were effectively controlled with minimal side effects—providing crucial insights for future clinical practice.
Bao Chunde hopes this research will yield a widely accessible treatment for refractory LN patients, enhancing their quality of life. He remains committed to refining strategies and pursuing further breakthroughs.
“For the future, we are optimistic. Through our efforts, we aim to validate more therapies for clinical use, bringing hope to patients. We will also continue investigating novel drugs, striving for transformative advances in the near term.”
Beyond lupus and common rheumatic diseases, Bao Chunde has also focused on rare conditions.
Amyopathic dermatomyositis-associated interstitial lung disease (ADM-ILD) is a severe rheumatic disorder. Patients often experience rapid progression, leading to respiratory failure and mortality rates as high as 70%. Though not extremely common, ADM-ILD is relatively frequent at Renji Hospital, a center specializing in rheumatology. Characterized by distinct skin manifestations and rapid-onset interstitial pneumonia, it poses a grave threat.
“Initially, the medical community lacked understanding of this condition, and existing treatments were ineffective. Facing such high mortality, clinicians felt nearly powerless. In 2012, I recruited a PhD student specializing in respiratory medicine to launch joint research. We began with a systematic analysis of clinical cases and established a dedicated research platform—a pivotal step forward.”
Bao Chunde’s work opened new therapeutic avenues for ADM-ILD, markedly improving survival rates. Their cumulative efforts built a systematic research framework, laying the groundwork for future studies.
As Bao Chunde often says, “Research drives progress.” Their endeavors have brought tangible change to treating this rare disease.
The department’s research also encompasses risk assessment and treatment response. After analyzing extensive clinical data, the team developed the Frames Model, a novel predictive tool. This model enables physicians to forecast disease severity based on individual patient profiles, facilitating personalized treatment strategies.
“In exploring new therapies, we moved beyond the limitations of conventional immunosuppressants like high-dose steroids. We trialed novel agents such as calcineurin inhibitors, achieving significantly better outcomes. The introduction of iguratimod—aligned with our pathogenesis research—was particularly impactful, dramatically reducing mortality from the once-dreaded 70% rate.”
Bao Chunde’s achievements in ADM-ILD have drawn medical attention to this rare disease, transforming it from an insurmountable challenge into a manageable condition through scientific innovation and novel therapeutics.
“I once consulted on a middle-aged female patient presenting with headaches, low-grade fever, and kidney dysfunction. Despite seeing specialists across multiple departments, she remained undiagnosed. Through detailed examination and renal biopsy, we confirmed SLE affecting her nervous system, kidneys, and blood. With a clear diagnosis, her treatment progressed successfully.”
This experience reinforced Bao Chunde’s view that modern medicine’s overspecialization can hinder care for complex, multi-system diseases. He advocates for a more integrated approach to medicine to better address such challenges.

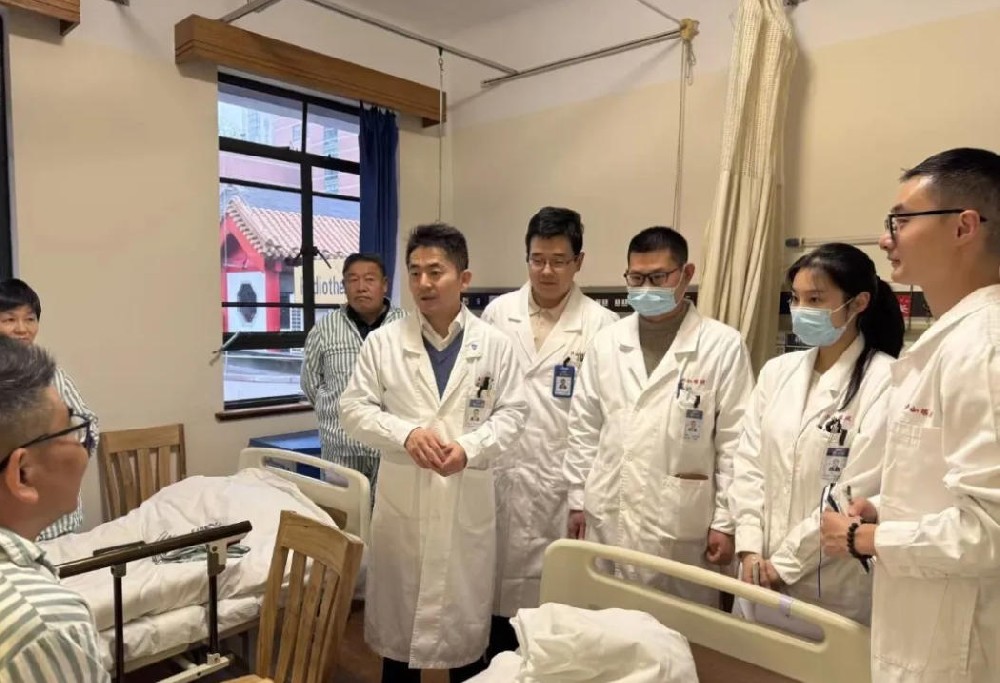
Mentoring the Next Generation
As a PhD supervisor, Bao Chunde’s mentorship extends beyond research, emphasizing the integration of clinical practice and scientific innovation to cultivate well-rounded abilities. He instills the principle of “respecting patients” as the core of medical practice—a philosophy deeply embedded in his teaching.
“As a mentor, I prioritize cultivating problem-oriented thinking in students. Our department engages in both basic and clinical research. Basic science explores disease mechanisms, while clinical research addresses patient needs. Students must therefore identify research questions from patient challenges and strive to solve them.”
Bao Chunde views clinical practice as the wellspring of research. He advocates identifying problems in patient care and using them as research starting points. This ensures studies have practical relevance while driving clinical progress. He stresses that students’ research must meaningfully advance clinical practice—not merely serve academic publication.
Renji’s rheumatology department is divided into two branches: one focused on basic research, the other on clinical studies. Clinical research not only solves specific medical problems but also propels broader clinical advancements. Collaborations with institutions like the Chinese Academy of Sciences provide students with hands-on training in experimental techniques. Bao Chunde encourages engagement in both domains to foster comprehensive development.
Another key aspect of his mentorship is shaping students’ mindset and capabilities. He promotes integrity, humility, and continuous learning through practice, believing these traits underpin true success in research and clinical work.
“In mentoring, I emphasize foundational knowledge. Students need solid basics to progress lifelong. In research, we prioritize practical outcomes. New methods and technologies must align with clinical needs; otherwise, research becomes detached. Our goal is for students to accumulate experience and apply it meaningfully.”
Bao Chunde upholds the principle of “benevolent skill,” believing a physician’s duty lies not just in technical excellence but in genuine patient care. This ethos permeates his practice and teaching. He insists doctors must fully commit to diagnosis and treatment, leaving no room for complacency.
He holds physicians to the highest standards, emphasizing meticulous attention to detail—especially in avoiding unnecessary tests and treatments. He urges medical professionals to uphold ethical integrity, preserving patient trust by avoiding overtreatment.
“I often remind my team that patients come to us after exhausting other options. We must offer our best expertise and service. In clinics, I thoroughly assess each patient to ensure optimal care. I also critique excessive testing and treatment within the hospital, advocating for reform.”
For decades, Bao Chunde has bridged medical research and clinical practice to solve real-world problems. He prioritizes foundational knowledge and practical skills while demanding physicians meet the “dual standards” of technical mastery and compassionate care. For the medical field, he calls for reduced overtreatment, emphasizing standardization and improvement.
Looking ahead, he aims to drive further progress through research innovation, educational excellence, patient-centered care, and systemic reform—paving the way for new milestones at Renji Hospital’s Department of Rheumatology.
Editor: Chen Qing @ ShanghaiDoctor.cn
Note: Chinese Sources from “The Path of Benevolent Medicine” which was published in 2024. It records 90 important medical figures in the history of Renji Hospital. Yewen Renyi (ShanghaiDoctor.cn) team was one of the major writers of the book and is authorized by Renji hospital to create English version on the website of ShanghaiDoctor.cn
Hospital: Renji Hospital, Shanghai Jiao Tong University School of Medicine
Dr. Zou Shien | A Physician’s Mission in Gynecological World
Dr. Bao Shihua | Where Dreams Begin from Reproductive Immunology
Dr. Yang Zhigang | The Art of the Healer: Between the Brush and the Brain
Dr. Cai Junfeng | Guarding Bone and Joint Health, Improving Quality of Life
Dr. Xu Xiaosheng|The Gentle Resilience of a Male Gynecologist
Dr. Shi Hongyu | A Cardiologist with Precision and Compassion
Dr. Zhang Guiyun|The Inspiring Path of a Lifesaving Physician

Dr. Zou Shien | A Physician’s Mission in Gynecological World

Dr. Cui Song | Healing the Heart, in Every Sense

Dr. Bao Shihua | Where Dreams Begin from Reproductive Immunology
Dr. Yang Zhigang | The Art of the Healer: Between the Brush and the Brain
Dr. Zhou Qianjun | Sculpting Life in the Chest

Dr. Cai Junfeng | Guarding Bone and Joint Health, Improving Quality of Life

Dr. Cui Xingang | The Medical Dream of a Shanghai Urologist

Dr. Xu Xiaosheng|The Gentle Resilience of a Male Gynecologist

Dr. Shi Hongyu | A Cardiologist with Precision and Compassion

Dr. Zhang Guiyun|The Inspiring Path of a Lifesaving Physician