Update time:2025-10-02Visits:3999

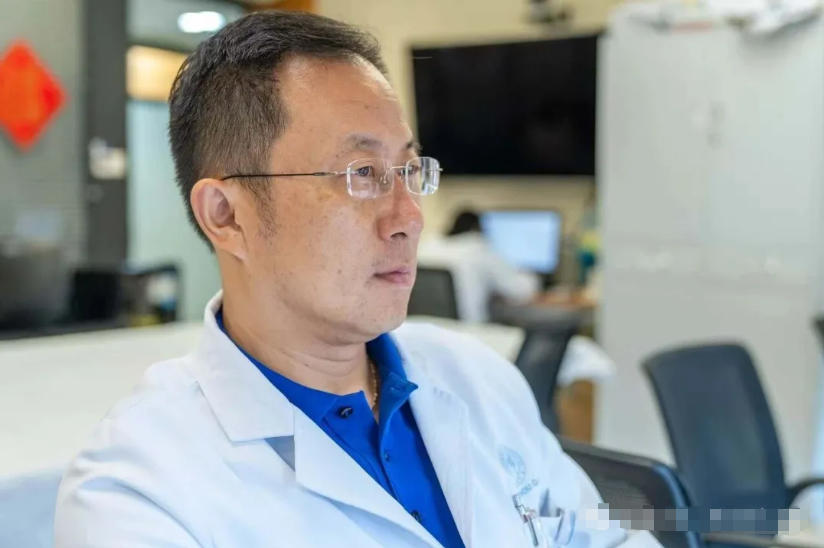
Gastroenterology Professor, Deputy Director of the Shanghai Institute of Digestive Diseases, Chief Physician, Department of Gastroenterology, Renji Hospital
Introduction
Hailing from a family with a seven-generation legacy in medicine, he inherited a profound tradition of medical ethics and compassion. With unwavering focus and dedication, he has committed his career to navigating the vast and complex field of medicine, constantly pushing the boundaries of what is possible.
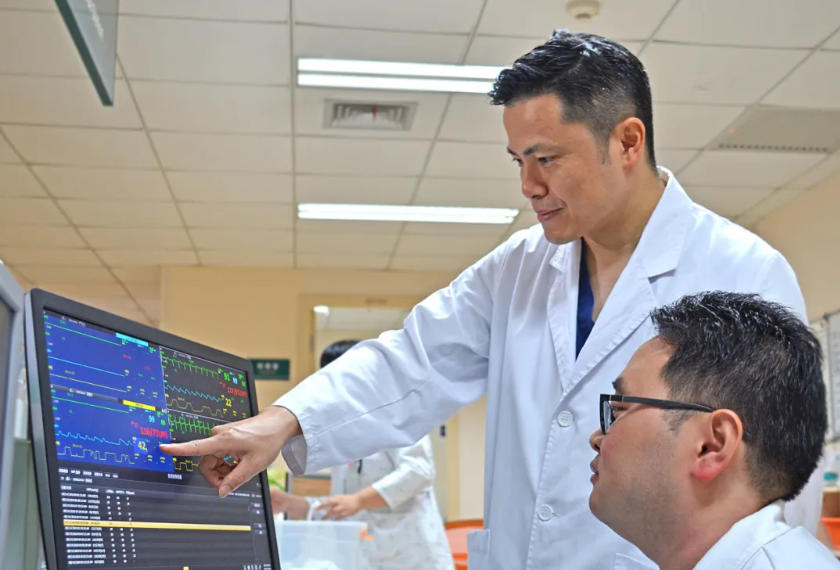
He has never shied away from a challenge, particularly the small intestine—a notoriously difficult-to-access region of the digestive system. In the diagnosis and treatment of its diseases, he has been a true pioneer, developing innovations that transcend the limitations of traditional imaging. He spearheaded the clinical adoption of capsule endoscopy and balloon-assisted enteroscopy, making historic contributions to unveiling the mysteries of small bowel disorders.
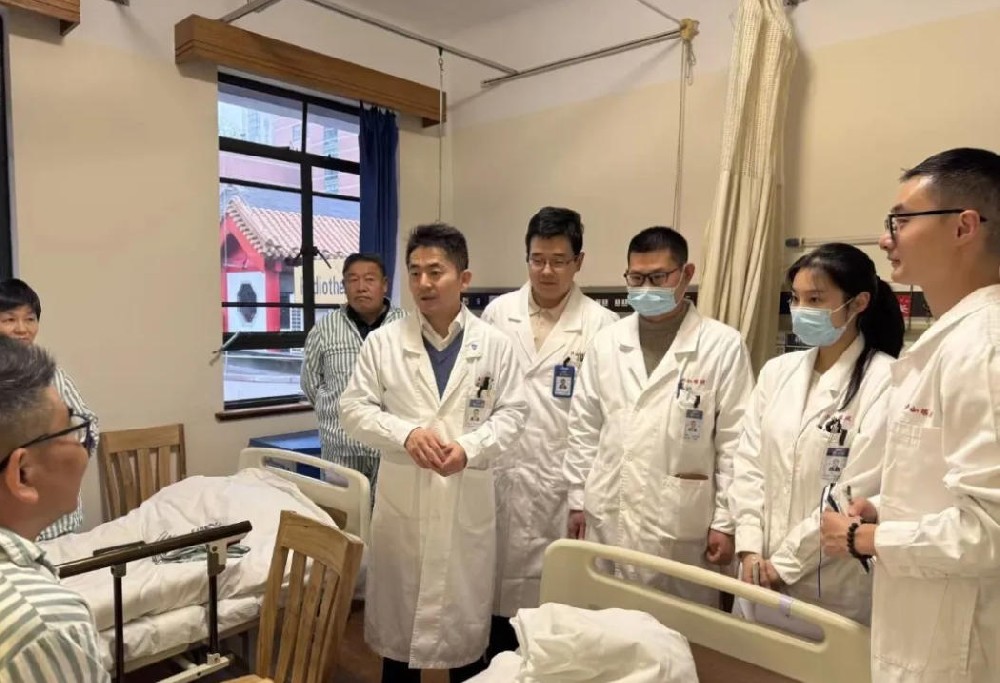
While treating patients on the front lines of clinical care, he is equally dedicated to mentoring the next generation of physicians. He recognizes that cultivating future talent is synonymous with shaping the future of the discipline itself.
He generously shares his extensive clinical experience and profound academic insights with young students, inspiring them to center their work on patients, to be driven by innovation, and to relentlessly pursue medical truth and excellence.
The Path to Medicine
“I come from a medical family; our lineage in healing spans seven generations. As a child, I often returned to my hometown, and I still vividly recall the art and atmosphere of Traditional Chinese Medicine (TCM). The practice of using ancestral medical knowledge to heal the community left a profound impression on me. Although my father chose to pursue business over medicine, discontinuing our family’s TCM practice, the medical tradition at home still deeply influenced me.”
In 1978, at the age of 18, Ge Zhizheng graduated from high school. This was a pivotal year in China’s history, marked by the new Reform and Opening-Up policy and the restoration of the National College Entrance Examination, known as the Gaokao. For his generation, this was a life-altering opportunity: the chance to finally choose their own destiny. Ge Zhizheng seized this once-in-a-lifetime opportunity and chose to pursue Western Medicine, applying to medical school.
“At the time, I felt that while TCM and Western Medicine are vastly different, their ultimate goal is the same: to treat illness and save lives. Different paths to the same destination.”
After successfully enrolling at Shanghai Second Medical College (now part of Shanghai Jiao Tong University School of Medicine), Ge Zhizheng thrived, driven by his passion for medicine and meticulous nature.
“Shanghai Second Medical College was already an excellent institution back then,” he recalls. “I felt incredibly fortunate to study there. It provided me with a solid foundation in medical knowledge. As a medical student, I began my internship at Renji Hospital, rotating through various departments where I gained invaluable practical skills.”
During his internship at Renji Hospital, Ge Zhizheng worked alongside many distinguished senior physicians. It was during this period that he began to contemplate his future and discovered a particular affinity for gastroenterology.
“The Department of Gastroenterology at Renji Hospital had a prestigious legacy and a rigorous academic atmosphere,” he remembers. “I recall during my rotations meeting Academician Jiang Shaoji and Professor Xiao Shudong. These two incredibly scholarly and distinguished individuals had made outstanding contributions to the field. Their personal charisma and the department’s culture deeply attracted me.”
Although formal national rankings for medical specialties didn’t exist at the time, Renji Hospital’s Gastroenterology Department was already renowned throughout the country. Ge Zhizheng decided to build his career there.
He understood that a strong platform is crucial for professional growth, and Renji’s department provided the ideal stage for him to showcase his talents and advance in the field. During this period, he chose to pursue advanced studies.
“It was then I decided to pursue my Master’s and doctoral degrees,” he says. “Professor Xiao Shudong was my supervisor for both. Under his guidance, I not only acquired a solid foundation of medical knowledge but also learned principles for conducting myself with integrity. Professor Xiao’s approachable nature and noble character benefited me immensely, both academically and personally.”
Professor Xiao Shudong was a towering figure in Chinese gastroenterology, known for his breakthroughs in diagnosing and treating digestive diseases and his remarkable contributions to developing new talent. He was a driving force behind the advancement of the discipline in China. Ge Zhizheng solidified his foundation during his postgraduate studies. The academic environment at Renji Hospital’s Gastroenterology Department and the Shanghai Institute of Digestive Disease—co-founded by Academician Jiang Shaoji and Professor Xiao Shudong—was instrumental in his development. It provided a robust foundation for his future research and clinical practice, enhancing his influence both within China and internationally.
The Hidden Challenge of Small Intestinal Diseases
The small intestine, a winding organ several meters long, has long been an elusive “black box” within the digestive system. As most of its length lies beyond the reach of traditional gastroscopes and colonoscopes, it was considered a “blind spot” for endoscopists. Furthermore, its constant peristalsis poses a significant challenge for any instrument attempting to navigate its path.
“In medical research, the small intestine has always been a difficult frontier to conquer. In the past, our medical understanding of it was almost a blank slate. Many cases of small intestinal bleeding couldn’t be traced to a clear cause and were labeled ‘obscure,’ presenting a tremendous challenge for both patients and physicians.”
In earlier years, diagnosing small intestinal diseases was fraught with difficulty due to the limitations of traditional imaging. First, these techniques typically offered only rough, indirect observations, making it difficult to accurately diagnose early or minute lesions, such as small submucosal vascular abnormalities. Second, inflammatory bowel diseases like Crohn’s disease often begin with subtle mucosal erosions or small ulcers, which were equally hard to detect with imaging. Early-stage tumors, especially those smaller than 1 cm, were challenging to spot due to the intestine’s tortuous structure, where they could be obscured by the natural overlapping of bowel loops.
The clinical introduction of capsule endoscopy in 2001 and double-balloon enteroscopy in 2003 transformed the diagnosis and treatment of small intestinal diseases, ending a long-standing era of clinical uncertainty. This was a landmark achievement. As one of the first units in China to adopt these technologies, the Gastroenterology Department of Renji Hospital held a significant technological advantage. Marking the dawn of the small bowel endoscopy era, Professor Ge Zhizheng and his team embarked on a journey of exploration into the diagnosis and treatment of small intestinal diseases that has now spanned over two decades. In the field of small intestinal bleeding—the “final blind spot” of the digestive tract—he has led his team in conducting dozens of innovative clinical studies over the past 20 years. These efforts not only significantly improved the diagnostic rate for small intestinal diseases but also resulted in findings cited by 24 international guidelines or expert consensus statements. His pioneering protocol using thalidomide to treat bleeding from small intestinal angiodysplasia even rewrote international guidelines. He revealed key pathogenic mechanisms and established a robust chain of evidence-based medicine for treating gastrointestinal vascular malformation bleeding, achieving a major breakthrough in clinical history. His research findings were published in the prestigious New England Journal of Medicine (NEJM). This “Chinese solution” he proposed tackles a global challenge, fills a therapeutic void for this stubborn condition, and brings Chinese experience to the forefront of global health. He has become a true “pioneer” and “leader” in the field.
“In practical application, we quickly realized that merely possessing new technology was far from sufficient. To truly unlock their potential, we had to continuously explore and optimize related operational procedures. For instance, during capsule endoscopy, how to effectively prepare the intestine for clearer internal observation was a major challenge. Through extensive clinical trials, we proposed systematic bowel preparation protocols and studied different dosages and timings of cleansing agents, ultimately establishing suitable operational standards. These research outcomes gained broad international recognition and were published in several top-tier medical journals.”
Building on the capabilities of capsule endoscopy and enteroscopy, the team has conducted a series of studies over 20 years to improve the diagnostic rate for small intestinal diseases. They have proposed numerous significant findings that were first discovered and confirmed in China and internationally, such as the study published in the authoritative journal GUT on improving the diagnosis and treatment of small intestinal diseases, and a series of studies on standardizing pre-examination preparation to enhance capsule endoscopy diagnostic rates. In total, they published 57 related papers, with research findings cited by 24 international guidelines or expert consensus statements, highlighting their significant clinical impact. In 2008, he led the development of China’s first “Clinical Practice Guidelines for Capsule Endoscopy”; in 2014, he spearheaded the revision of the second edition; and in 2023, he led the formulation of China’s first “Chinese Expert Consensus on Endoscopic Diagnosis and Treatment of Small Intestinal Bleeding,” laying a solid foundation for subsequent clinical treatments.

From Diagnosis to Cure: The Ultimate Goal
Professor Ge Zhizheng’s team recognized that diagnosis was only the first step; the ultimate goal was treatment. As diagnostic capabilities improved, the true challenges in treating small intestinal diseases became apparent. Clinical studies show that these diseases most commonly manifest as gastrointestinal bleeding (over 60% of cases), with vascular malformations, or angiodysplasia, being the most frequent cause (over 50%). These lesions are often deep-seated, hidden, multiple, and recurrent, making endoscopic or surgical treatments difficult. With virtually no effective pharmacological options available, this created a major clinical challenge.
Gastrointestinal Involvement in Vascular Malformations (GIVM) is a distinct condition marked by thin-walled, immature vessels that are often hidden, multiple, and recurrent. Approximately 50% of patients require repeated hospitalizations or rely on regular blood transfusions, severely impacting their quality of life and placing a heavy burden on both their families and society.
Recurrent bleeding from small intestinal angiodysplasia accounts for 5-10% of all gastrointestinal bleeding and predominantly affects elderly patients. Past treatments offered little hope. Hormone therapy, used in the 1980s and 90s, was proven ineffective and unsafe in a 2001 trial and was subsequently abandoned. While some observational studies suggested somatostatin analogs might help, their efficacy remains unproven and recurrence rates are high. Invasive options like embolization or surgery also frequently fail because the lesions are numerous, hard to locate, and spread throughout the intestine’s complex 5-7 meter length. Furthermore, many elderly patients cannot tolerate the risk of these procedures. For decades, this condition persisted with no reliable treatment and no specific drugs.
The search for a safe and effective drug became a critical global priority. In 2003, after a comprehensive review of international literature, the team hypothesized that thalidomide—known for its anti-angiogenic properties—could be an ideal treatment for bleeding from angiodysplasia. Though once used for morning sickness, its later-discovered medical effects suggested a new purpose, offering a potential “new lease on life” for this decades-old drug.
This led to a long-term, methodical research journey. Starting in 2003, the team systematically investigated thalidomide’s potential, progressing from initial case analyses to clinical observational studies and, in 2011, a pivotal randomized open-label study published in Gastroenterology. These early studies provided crucial insights into the drug’s efficacy, dosage, and safety, leading to its inclusion as a recommended treatment in the 2015 American College of Gastroenterology guidelines.
The final, decisive step was a large-scale, randomized double-blind placebo-controlled trial (RCT)—the gold standard in clinical research. In 2015, the team secured crucial funding from Shanghai Jiao Tong University School of Medicine’s Highland and Peak Discipline Development Initiative, which was designed to foster research-oriented physicians and drive innovation at the patient’s bedside.
With this support, Professor Ge’s team launched and successfully completed the world’s first investigator-initiated, multicenter, double-blind, placebo-controlled RCT to determine the long-term efficacy and safety of thalidomide for this condition. The results were definitive: thalidomide significantly reduced recurrent bleeding. This landmark finding was published as an original article in the prestigious New England Journal of Medicine (NEJM)—a first for China’s gastroenterology field. The research results fill a critical therapeutic void for this disease.
Led by Professor Ge as corresponding author, the study was a major collaboration involving 10 leading tertiary hospitals across China, with key contributions from Dr. Chen Huimin and Dr. Wu Shan. The project was funded by the Shanghai Highland and Peak Discipline Development Initiative, the National Natural Science Foundation of China, and the Shanghai Shenkang Hospital Development Center.
The international impact was immediate. Dr. Loren Laine, Chair of the Department of Gastroenterology at Yale University, wrote an accompanying editorial in the NEJM, stating that the study “provides evidence… of higher quality than any other evidence for this indication.”
“Our research has gained widespread recognition,” the team noted. “This discovery represents a successful case of drug repurposing and, more importantly, a significant contribution to medical research and clinical practice.”
For Professor Ge, this success is not an endpoint, but a beginning. Many challenges remain, and the team is committed to further innovation. “The vitality of clinical research,” he believes, “lies in its origin from practice, long-term focus, and unwavering persistence.”
To date, Professor Ge’s team has published 57 papers from this research line, with their findings being incorporated into 41 international guidelines. This work has not only had a profound impact on patient care but has also significantly elevated the international standing of Chinese medicine in the field of small intestinal diseases.

Nurturing Talent and Forging the Future of Medicine
For Ge Zhizheng, education and teaching are an indispensable part of his career. Educating the next generation is not merely about transmitting knowledge; it’s about shaping the future standard of healthcare. As a professor, he excels at balancing the demanding dual roles of clinician and educator.
“First and foremost, time management is paramount. Medical work is busy and complex, requiring an orderly schedule. I typically create detailed work plans, striking a reasonable balance between my professional and personal life. For instance, I prioritize tasks based on urgency, tackling the most critical ones first. I also maintain a clear personal schedule to ensure I can dedicate quality time to my family and my own interests.”
In medical education, an educator must possess deep expertise, excellent communication skills, and effective teaching techniques. The ability to distill complex medical concepts into clear, accessible lessons is a crucial skill for every medical educator. Simultaneously, balancing personal life and work is essential for ensuring teaching quality and the educator’s own well-being.
“I find communication skills to be particularly important. A student’s ability to understand and master medical knowledge often hinges on effective communication. In the classroom, I strive to explain complex medical concepts using vivid case studies and simple language to help students grasp and retain the information more effectively.”
Ge Zhizheng also recognizes that maintaining a healthy lifestyle is vital for effective teaching. Adequate sleep, a balanced diet, and regular exercise not only boost work efficiency but also keep his mind sharp and his energy high during lectures. He avoids unnecessary social engagements, dedicating more time to his family and activities he enjoys, such as listening to classical music and traveling.
In the world of medical education, personal hobbies and lifestyle are more than just a way to unwind; they are crucial for boosting productivity and sparking creativity. A healthy work-life balance helps physicians maintain their physical and mental health, enabling them to be more engaged and effective as educators.
“I personally love classical music. Every day after work, I listen to music for a while; it helps me relax. Traveling and photography are also my hobbies. I arrange a trip each year, allowing me to step away from the busy work routine and recharge. Through these hobbies, I maintain a positive mindset and creative inspiration.”
For young physicians, finding balance amidst a demanding workload, managing time effectively, and maintaining a healthy lifestyle are challenges that require serious attention. He believes that sharing these experiences can help them better adapt to the rigors of the medical profession and find fulfillment in their personal lives.
“My advice to young doctors is, first, learn to manage your time effectively. Create clear work plans and schedules to ensure you allocate time efficiently between work and personal life. Learn to say ‘no’ and avoid taking on tasks that exceed your capacity. Second, maintain good lifestyle habits—prioritize sufficient sleep and a healthy diet, as this is crucial for improving both your work efficiency and your quality of life. Finally, and most importantly, maintain focus in everything you do, whether at work or in life. Be fully present in your work, but also learn to savor the small joys of life. When you are working, devote yourself completely; when you are living, enjoy it fully. Only by doing so can you achieve true success in your career and find happiness in your life.”
Looking ahead, Ge Zhizheng is focused and optimistic.
“Currently, I am focused on several key areas. First, I am committed to continuously enhancing my clinical skills. Medicine evolves rapidly, and I want to remain at the forefront of new knowledge and constantly improve my abilities in practice. Second, I am deeply interested in medical innovation and translating research into clinical practice, especially at the intersection where medical research meets patient care. I hope to participate in more research projects that explore new treatments and technologies. Innovation isn’t just about technological breakthroughs; it’s about making tangible contributions to patient health. I want to work with my team to translate our research findings into clinical applications that provide patients with better treatment options.”
In a rapidly changing medical environment, questions of how to maintain foresight, adapt to new developments, and drive medical progress through education and research are ones every physician must grapple with. Ge Zhizheng believes that only through continuous learning and innovation can physicians achieve career success, contribute to the advancement of medicine, and further elevate the Renji Hospital’s Gastroenterology Department.
Editor: Chen Qing @ ShanghaiDoctor.cn
If you'd like to contact to Dr Ge, please be free to email us at chenqing@ShanghaiDoctor.cn for any help.
Note: Chinese Sources from “The Path of Benevolent Medicine” which was published in 2024. It records 90 important medical figures in the history of Renji Hospital. Yewen Renyi (ShanghaiDoctor.cn) team was one of the major writers of the book and is authorized by Renji hospital to create English version on the website of ShanghaiDoctor.cn
Hospital: Renji Hospital, Shanghai Jiao Tong University School of Medicine
Dr. Liang Wei | Dedicated to Vascular Health, Safeguarding the Body’s Lifelines
Dr. Zou Shien | A Physician’s Mission in Gynecological World
Dr. Bao Shihua | Where Dreams Begin from Reproductive Immunology
Dr. Yang Zhigang | The Art of the Healer: Between the Brush and the Brain
Dr. Cai Junfeng | Guarding Bone and Joint Health, Improving Quality of Life
Dr. Xu Xiaosheng|The Gentle Resilience of a Male Gynecologist
Dr. Shi Hongyu | A Cardiologist with Precision and Compassion
Dr. Liang Wei | Dedicated to Vascular Health, Safeguarding the Body’s Lifelines

Dr. Zou Shien | A Physician’s Mission in Gynecological World

Dr. Cui Song | Healing the Heart, in Every Sense

Dr. Bao Shihua | Where Dreams Begin from Reproductive Immunology
Dr. Yang Zhigang | The Art of the Healer: Between the Brush and the Brain
Dr. Zhou Qianjun | Sculpting Life in the Chest

Dr. Cai Junfeng | Guarding Bone and Joint Health, Improving Quality of Life

Dr. Cui Xingang | The Medical Dream of a Shanghai Urologist

Dr. Xu Xiaosheng|The Gentle Resilience of a Male Gynecologist

Dr. Shi Hongyu | A Cardiologist with Precision and Compassion